Fill in Your Annual Physical Examination Template
Documents used along the form
When preparing for an annual physical examination, various forms and documents may be required to ensure a comprehensive assessment of an individual's health. Each of these documents serves a specific purpose in gathering important information about the patient's medical history, current health status, and any ongoing treatments or medications. Below is a list of commonly used forms that complement the Annual Physical Examination form.
- Medical History Form: This document collects detailed information about the patient's past medical history, including previous illnesses, surgeries, and family health history. It helps healthcare providers understand potential risk factors and tailor their assessments accordingly.
- Medication List: A comprehensive list of all medications currently being taken by the patient, including over-the-counter drugs and supplements. This helps avoid potential drug interactions and ensures that the healthcare provider is aware of all substances affecting the patient's health.
- Immunization Record: This form outlines the patient's vaccination history, including dates and types of vaccinations received. It is essential for tracking immunizations and ensuring that the patient is up to date on necessary vaccines.
- Consent for Treatment Form: This document provides consent for the healthcare provider to perform examinations, tests, and treatments. It ensures that the patient understands and agrees to the procedures being conducted during the visit.
- Referral Form: If a specialist consultation is needed, this form is used to refer the patient to another healthcare provider. It includes details about the patient's condition and the reason for the referral.
- Disciplinary Actions Disclosure: For individuals in real estate, understanding the importance of the arizonaformspdf.com/ is essential when applying or renewing licenses, as it reveals any past disciplinary issues that may influence licensing decisions.
- Patient Information Sheet: This sheet collects essential personal information, such as contact details, insurance information, and emergency contacts. It is crucial for administrative purposes and to facilitate communication.
- Health Questionnaire: This form may include questions about lifestyle habits, such as diet, exercise, smoking, and alcohol consumption. It provides insight into the patient's daily habits and helps identify areas for improvement.
- Lab Test Requisition Form: If lab tests are required, this form is used to request specific tests from a laboratory. It includes details about the tests needed and the patient's information to ensure accurate processing.
- Follow-Up Care Plan: After the examination, this document outlines any recommended follow-up actions, including additional tests, referrals, or lifestyle changes. It serves as a guide for the patient to maintain or improve their health.
Each of these forms plays a vital role in ensuring that healthcare providers have the necessary information to deliver effective care. By completing these documents accurately, patients can help facilitate a smooth and thorough annual physical examination process.
More PDF Templates
How Do You File a Mechanics Lien - In some cases, lien releases are required if negotiations are successful.
In addition to facilitating the sale, the Oklahoma Motor Vehicle Bill of Sale form can be conveniently accessed through platforms offering Auto Bill of Sale Forms, ensuring that sellers and buyers have the necessary documentation to complete their transaction with clarity and confidence.
How to File a Construction Lien in Florida - This document is pivotal in establishing the timeline and communication regarding unpaid amounts.
Similar forms
The Annual Physical Examination form shares similarities with the Health History Questionnaire. Both documents collect essential personal information such as name, date of birth, and medical history. The Health History Questionnaire often includes questions about past illnesses, surgeries, and family medical history, which helps healthcare providers assess risk factors and tailor care accordingly. Like the Annual Physical Examination form, it emphasizes the importance of accurate and complete information to ensure effective medical evaluations.
The Immunization Record is another document akin to the Annual Physical Examination form. It serves to track vaccinations received by an individual over time. Both documents require details about immunizations, including dates and types administered. The Immunization Record is crucial for ensuring that patients are up-to-date with their vaccinations, just as the Annual Physical Examination form aims to review a patient's overall health status and preventive care needs.
The Medication List is comparable to the medication section of the Annual Physical Examination form. This document outlines all current medications, including dosages and prescribing physicians. Both forms stress the importance of accurately listing medications to avoid adverse drug interactions and ensure safe treatment plans. This comprehensive approach aids healthcare providers in making informed decisions about patient care.
The Consent for Treatment form also parallels the Annual Physical Examination form. Both documents require patient information and consent for medical evaluations and treatments. The Consent for Treatment form explicitly seeks permission for procedures, while the Annual Physical Examination form implicitly indicates consent through the completion of required information. This ensures that patients are informed participants in their healthcare journey.
The Referral Form is another similar document, particularly when a primary care physician refers a patient to a specialist. Like the Annual Physical Examination form, it includes patient demographics and relevant medical history. Both forms facilitate effective communication between healthcare providers, ensuring that specialists have the necessary background to provide appropriate care.
The Patient Registration Form shares commonalities with the Annual Physical Examination form. Both documents collect essential demographic information and medical history. The Patient Registration Form often serves as the initial point of contact in a healthcare setting, while the Annual Physical Examination form is focused on ongoing health assessment. Both are vital for establishing a comprehensive patient profile.
The Health History Questionnaire is a document that collects a patient's past medical history, lifestyle choices, and family health patterns. Like the Annual Physical Examination form, it aims to provide a comprehensive overview of health-related information. Patients typically fill out various sections regarding previous illnesses, surgeries, and medications. Additionally, both documents emphasize the importance of compiling a summary that can guide future medical treatment and preventive strategies. To ensure all legal paperwork is handled correctly, you can find the document here.
The Laboratory Test Requisition form is similar in that it collects necessary information for diagnostic testing. Both documents require patient details and often include sections for specific tests to be performed. The Laboratory Test Requisition form ensures that the right tests are ordered based on the patient's medical history, much like how the Annual Physical Examination form informs the necessary evaluations for overall health assessment.
Finally, the Emergency Contact Form shares similarities with the Annual Physical Examination form. Both documents collect crucial personal information, including emergency contacts and health conditions. The Emergency Contact Form is essential for ensuring that healthcare providers can quickly reach designated contacts in case of an emergency, while the Annual Physical Examination form provides a comprehensive overview of a patient's health status, which is equally important in urgent situations.
Steps to Filling Out Annual Physical Examination
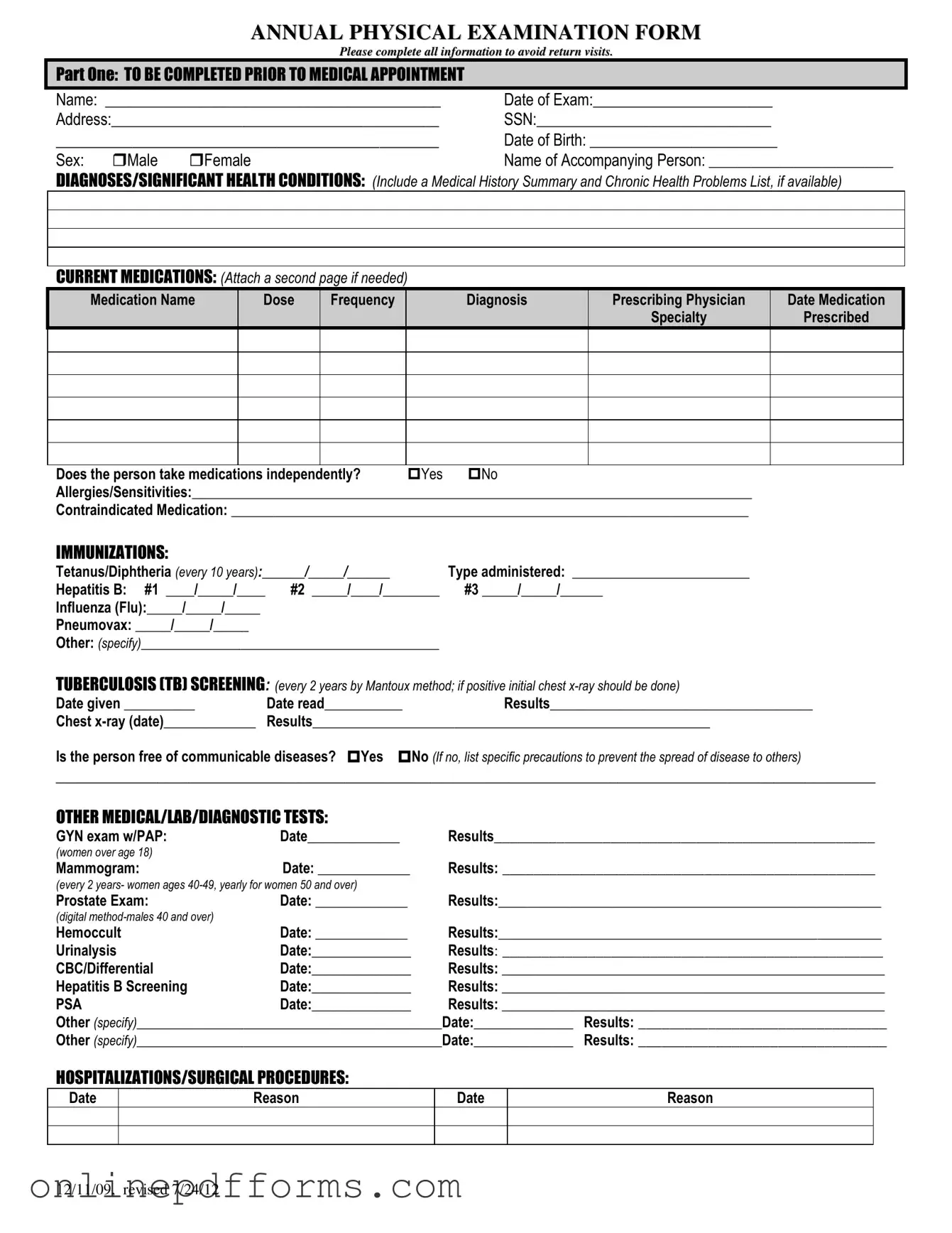
Completing the Annual Physical Examination form is essential for ensuring that your medical appointment goes smoothly. This form collects important health information that your healthcare provider will use to assess your health status and make recommendations. Follow these steps to fill out the form accurately.
- Personal Information: Fill in your name, date of exam, address, Social Security Number (SSN), date of birth, and sex. If applicable, include the name of the person accompanying you.
- Health History: Provide details about any significant health conditions and diagnoses. If you have a medical history summary or a list of chronic health problems, attach it.
- Current Medications: List all medications you are currently taking. Include the name, dose, frequency, diagnosis, prescribing physician, and date prescribed. Indicate whether you take medications independently and note any allergies or contraindicated medications.
- Immunizations: Record the dates and types of immunizations you have received, including Tetanus/Diphtheria, Hepatitis B, Influenza, and Pneumovax.
- Tuberculosis Screening: Document the date the TB test was given, the date it was read, and the results. If you have had a chest x-ray, include the date and results.
- Other Medical Tests: Fill in the dates and results for any other relevant medical or diagnostic tests, such as GYN exams, mammograms, prostate exams, and blood tests.
- Hospitalizations/Surgical Procedures: List any hospitalizations or surgeries, including the dates and reasons.
- General Physical Examination: Provide your blood pressure, pulse, respirations, temperature, height, and weight.
- Evaluation of Systems: For each body system listed, indicate whether the findings were normal and provide any additional comments or descriptions as necessary.
- Vision and Hearing Screening: Note whether further evaluation by a specialist is recommended for vision and hearing.
- Additional Comments: Include any recommendations for health maintenance, dietary instructions, limitations for activities, and any changes in health status from the previous year.
- Physician Information: At the end of the form, have your physician print their name, sign, and provide their address and phone number.