Fill in Your Prescription Pad Template
Documents used along the form
The Prescription Pad form is a crucial document in the healthcare system, facilitating the process of prescribing medication. However, it is often used in conjunction with several other forms and documents that ensure comprehensive patient care and adherence to legal standards. Below is a list of common documents that healthcare providers frequently utilize alongside the Prescription Pad form.
- Patient Intake Form: This document collects essential information about the patient, including medical history, allergies, and current medications. It helps healthcare providers understand the patient's background before making treatment decisions.
- Medication Administration Record (MAR): The MAR tracks all medications administered to a patient during their stay in a healthcare facility. It ensures accurate dosing and timing, promoting patient safety.
- Informed Consent Form: This form is used to obtain a patient's consent for specific treatments or procedures. It outlines the risks, benefits, and alternatives, ensuring that patients make informed decisions about their care.
- Referral Form: When a healthcare provider needs to send a patient to a specialist, a referral form is completed. This document includes relevant patient information and the reason for the referral, facilitating continuity of care.
- Insurance Authorization Form: This form is necessary for obtaining approval from insurance companies for specific treatments or medications. It helps ensure that the patient’s treatment will be covered financially.
- USCIS I-864 Form: This document is essential for sponsors seeking to financially support immigrants, demonstrating that they will not rely on government assistance. For more details, visit https://pdftemplates.info/uscis-i-864-form/.
- Lab Order Form: When tests or lab work are required, a lab order form is filled out. It specifies the tests needed and provides essential patient information to the laboratory.
- Discharge Summary: Upon a patient’s discharge from a healthcare facility, a discharge summary is created. It summarizes the patient’s treatment, medications prescribed, and follow-up care instructions.
- Follow-Up Appointment Schedule: This document outlines the recommended follow-up appointments for the patient. It helps ensure that ongoing care is coordinated and that patients do not miss critical check-ups.
These documents play an integral role in the healthcare process, enhancing communication among providers and ensuring that patients receive safe and effective care. Understanding their purpose and function can significantly improve the overall treatment experience.
More PDF Templates
Blank Direct Deposit Form - This method of payment is becoming increasingly popular among employers.
When it comes to documenting tractor transactions, having a reliable reference is crucial. The comprehensive Florida Tractor Bill of Sale template can guide parties through the necessary details of the sale while ensuring compliance with legal standards. For more information, visit this useful Tractor Bill of Sale reference.
Puppy Health Record - Document the birth date and time to understand development stages.
Similar forms
The Prescription Pad form is quite similar to a Medical Record. Both documents serve as essential tools for healthcare providers to track patient information and treatment plans. A Medical Record contains comprehensive details about a patient's medical history, treatments, and medications. Just like a Prescription Pad, it is crucial for ensuring continuity of care, allowing different healthcare professionals to access and understand a patient's treatment journey. Both documents emphasize the importance of accurate and timely documentation in the healthcare process.
The Texas Trailer Bill of Sale form is a vital document for anyone involved in the transaction of trailers in Texas, ensuring that all details of the sale are recorded clearly. Alongside other documents like the Auto Bill of Sale Forms, it plays a critical role in confirming the sale and transferring ownership, thereby streamlining the buying and selling process for trailers.
Another document that shares similarities with the Prescription Pad is the Medication Administration Record (MAR). This record is used in healthcare settings to document the administration of medications to patients. Like the Prescription Pad, the MAR includes details about the medication, dosage, frequency, and the healthcare provider's signature. Both documents aim to ensure that patients receive the correct medications at the right times, minimizing the risk of errors in medication administration.
The Treatment Plan is another document that parallels the Prescription Pad. A Treatment Plan outlines the strategies and interventions a healthcare provider intends to use for a patient’s specific health issues. Similar to how a Prescription Pad lists prescribed medications, a Treatment Plan may detail therapeutic approaches, lifestyle changes, and follow-up actions. Both documents are vital for guiding patient care and ensuring that treatment aligns with the patient’s needs and goals.
Patient Consent Forms also share a connection with the Prescription Pad. These forms are designed to obtain a patient's permission before proceeding with treatments or medications. Just as a Prescription Pad requires a healthcare provider's signature to validate a prescription, Patient Consent Forms necessitate a patient's signature to confirm their understanding and agreement to the proposed treatment. Both documents protect the rights of patients and ensure informed decision-making in healthcare.
Similarly, the Referral Form is akin to the Prescription Pad in that it facilitates communication between healthcare providers. A Referral Form is used when a primary care physician sends a patient to a specialist for further evaluation or treatment. Like the Prescription Pad, it contains important patient information and specific instructions for the receiving provider. Both documents play a crucial role in coordinating patient care and ensuring that all providers are on the same page regarding treatment plans.
The Lab Order Form is another document that mirrors the Prescription Pad. This form is used by healthcare providers to request laboratory tests for their patients. Just as a Prescription Pad specifies medications, a Lab Order Form details the tests to be conducted, along with relevant patient information. Both documents are essential for diagnosing and monitoring health conditions, ensuring that patients receive appropriate and timely testing.
In addition, the Discharge Summary is similar to the Prescription Pad in its role in patient care continuity. A Discharge Summary provides a comprehensive overview of a patient’s hospital stay, including treatments received and follow-up care instructions. Like the Prescription Pad, it is critical for ensuring that patients understand their ongoing care needs after leaving a healthcare facility. Both documents are key in facilitating smooth transitions between different levels of care.
Lastly, the Insurance Authorization Form shares similarities with the Prescription Pad. This form is used to obtain approval from an insurance company before certain treatments or medications are provided. Just as a Prescription Pad must be properly filled out to ensure a medication is dispensed, an Insurance Authorization Form must be completed accurately to secure coverage for medical services. Both documents are vital in navigating the complexities of healthcare and ensuring that patients receive necessary treatments without financial barriers.
Steps to Filling Out Prescription Pad
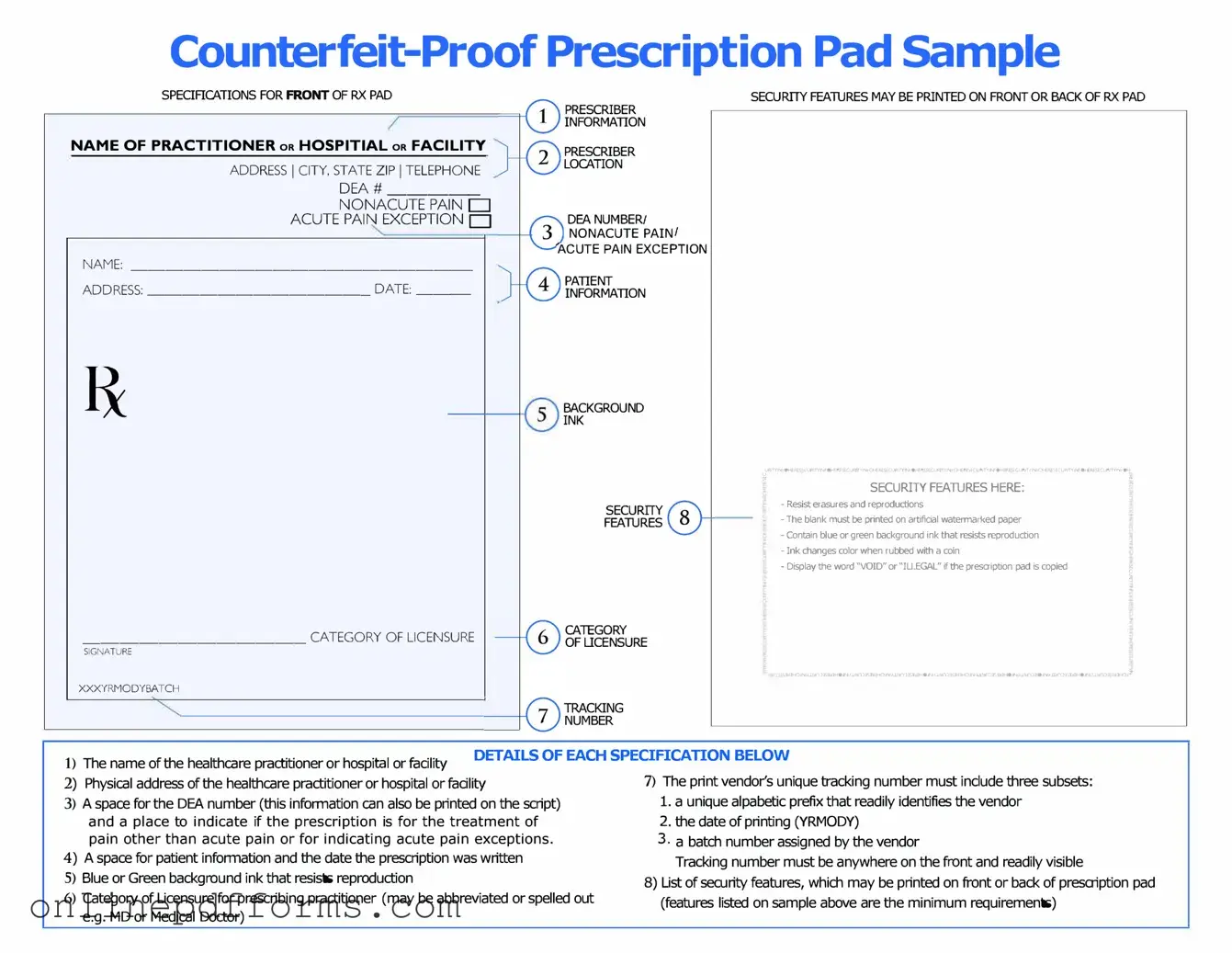
Completing the Prescription Pad form is a straightforward process that requires careful attention to detail. Once filled out correctly, this form will facilitate the necessary steps for obtaining medication. Follow these steps to ensure accuracy and clarity.
- Gather necessary information: Collect the patient's full name, date of birth, and contact information.
- Enter the date: Write the date on which the prescription is being issued.
- Fill in the medication details: Clearly specify the name of the medication, dosage, and frequency of administration.
- Indicate the quantity: Write the total number of units to be dispensed.
- Provide refills: If applicable, indicate the number of refills authorized.
- Sign the form: The prescribing physician must sign the form to validate it.
- Review the information: Double-check all entries for accuracy before submitting the form.