Fill in Your Tb Test Template
Documents used along the form
When undergoing a Tuberculosis (TB) test, several other forms and documents may accompany the TB Test form. These documents serve various purposes, from medical history to consent, ensuring a comprehensive understanding of the patient's health status and the testing process. Here’s a list of commonly used forms that you might encounter alongside the TB Test form:
- Medical History Form: This document collects detailed information about the patient's past medical conditions, surgeries, allergies, and medications. It helps healthcare providers assess any potential risks before administering the TB test.
- Informed Consent Form: Patients must sign this form to acknowledge that they understand the purpose of the TB test, the procedure involved, and any potential risks. This ensures that the patient is fully aware and agrees to proceed.
- Bill of Sale Form: This document serves as proof of ownership transfer for personal property. For more information, visit https://pdftemplates.info/washington-bill-of-sale-form/.
- Patient Identification Form: This form verifies the identity of the patient. It typically includes personal details such as name, date of birth, and contact information, ensuring accurate record-keeping and test results.
- Vaccination Record: A record of the patient's vaccination history may be required, particularly to check for any previous TB vaccinations. This helps healthcare professionals evaluate the patient's immune response.
- Referral Form: If the TB test is conducted as part of a larger medical evaluation, a referral form may be necessary. This document outlines the reasons for the test and any relevant medical history provided by the referring physician.
- Follow-Up Appointment Form: After the TB test is administered, a follow-up appointment may be scheduled. This form provides the details of the appointment, ensuring that the patient returns for results and further evaluation if needed.
- TB Screening Questionnaire: This questionnaire assesses the patient's risk factors for TB exposure and symptoms. It helps healthcare providers determine the necessity of the test and any immediate actions required based on responses.
- Results Notification Form: Once the TB test results are available, this form is used to communicate those results to the patient. It may also include recommendations for further action based on the outcome.
Understanding these accompanying documents can enhance your experience and ensure that you are well-informed throughout the TB testing process. Each form plays a vital role in providing thorough care and maintaining accurate health records.
More PDF Templates
How Many Cells in 96 Well Plate - Helps streamline sample processing with its 96-well format.
In addition to the required documentation, utilizing the correct forms is paramount for a smooth transaction; thus, many individuals opt for reliable resources like Auto Bill of Sale Forms to ensure compliance with Virginia's regulations during the sale of a trailer.
Is Geico Cheaper Than Progressive? - Confirm whether the vehicle is currently at the repair facility.
Similar forms
The TB Test form shares similarities with the Vaccine Administration Record (VAR). Both documents are used in healthcare settings to record critical information about a patient's vaccination status. The VAR includes details such as the patient's name, the vaccine administered, the date of administration, and the healthcare professional's signature. Like the TB Test form, the VAR requires completion of all sections to be considered valid, ensuring accurate tracking of immunizations.
The Florida Tractor Bill of Sale template is an important document that facilitates the transfer of ownership between a seller and buyer, ensuring that both parties are protected during the transaction. This form outlines essential details about the tractor, including its make, model, and identification numbers, while also capturing the signatures of both involved parties to validate the sale.
Another document akin to the TB Test form is the Allergy Action Plan. This form outlines a patient's allergies and the necessary actions to take in case of an allergic reaction. It includes sections for the patient's name, allergies, medications, and emergency contact information. Both forms emphasize the importance of accurate and complete information to provide effective care, as incomplete forms can lead to significant health risks.
The School Health Form also resembles the TB Test form in its purpose of documenting health-related information for students. This form typically includes sections for immunization records, health conditions, and parental consent. Both documents require signatures from healthcare professionals, ensuring that the information is verified and trustworthy, which is crucial for the safety of students in a school environment.
The Medical History Form is another document similar to the TB Test form. It collects comprehensive information about a patient's past medical conditions, surgeries, and family history. Like the TB Test form, it requires patients to provide detailed information to ensure that healthcare providers can make informed decisions about their care. Accurate completion of this form is essential for effective diagnosis and treatment.
The Consent for Treatment form is also comparable to the TB Test form. This document is used to obtain a patient's consent before administering medical treatments or procedures. It includes the patient's name, the procedure being consented to, and the signature of the healthcare provider. Both forms emphasize the need for informed consent, ensuring that patients understand the implications of the tests or treatments they undergo.
The Patient Registration Form shares similarities with the TB Test form in that it collects essential information about patients before they receive care. This form typically includes personal details, insurance information, and medical history. Both documents require thorough completion to facilitate effective communication between healthcare providers and patients, which is vital for delivering appropriate care.
The Health Assessment Questionnaire is another document that aligns with the TB Test form. It is used to gather information about a patient's current health status and any ongoing medical issues. Like the TB Test form, it requires patients to provide accurate information, as it directly impacts the quality of care they receive. Both forms aim to create a comprehensive picture of the patient's health for better treatment planning.
Lastly, the Laboratory Test Requisition form is similar to the TB Test form in that it is used to order specific tests for patients. This document includes patient identification, the tests requested, and the healthcare provider's signature. Both forms play a critical role in the diagnostic process, requiring precise information to ensure that the correct tests are performed and results are accurately interpreted.
Steps to Filling Out Tb Test
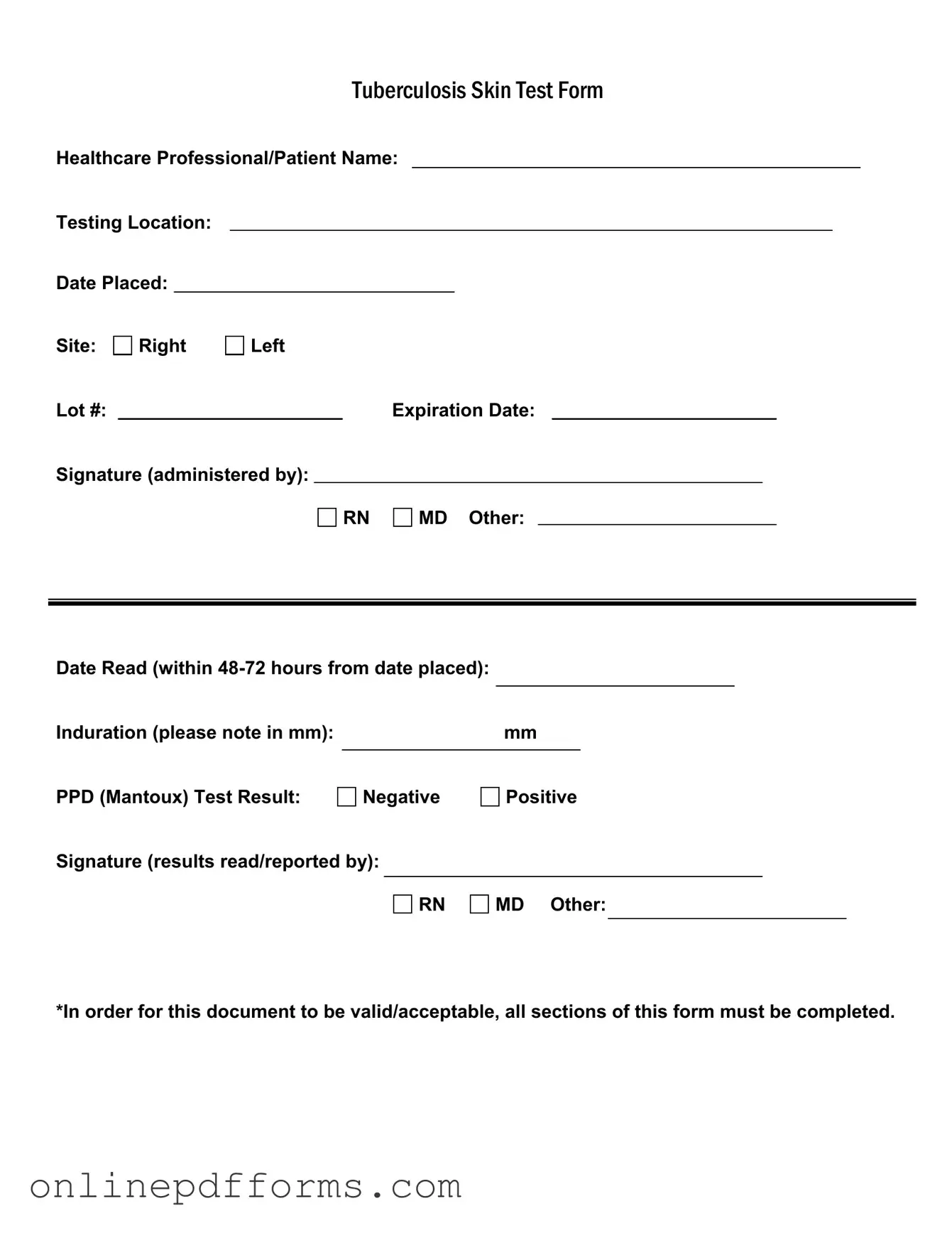
Completing the TB Test form accurately is essential for ensuring proper documentation of your test results. Follow these steps carefully to fill out the form correctly.
- Begin by entering the Healthcare Professional/Patient Name at the top of the form.
- Next, fill in the Testing Location where the test is being conducted.
- Record the Date Placed when the test was administered.
- Indicate the Site of the test by marking either Right or Left.
- Write down the Lot # of the PPD used for the test.
- Fill in the Expiration Date of the PPD.
- The Signature (administered by) section should be signed by the administering healthcare professional, choosing from RN, MD, or Other.
- Record the Date Read, which should be within 48-72 hours from the date placed.
- Measure and note the Induration in millimeters (mm).
- Indicate the PPD (Mantoux) Test Result as either Negative or Positive.
- Finally, the Signature (results read/reported by) should also be completed by the healthcare professional, selecting RN, MD, or Other.